Designing Medicines to Go Where They're Needed: Lessons from Liver Targeting
Designing transformational medicines for patients requires them to be efficacious and safe. Sometimes, drug molecules have the desired effect in the organ of treatment and undesired effects in other organs, meaning one way to achieve a safer medicine is through directing the drug molecule to the place it is needed and minimizing exposure in the rest of the body. When you take a medicine, how does it “know” exactly where to go in the body to provide a therapeutic effect and which organs to avoid where it may cause harm?
Scientists working in Medicine Design are constantly tackling this question. A new potential medicine may show great promise to treat a disease, but if it doesn’t reach its target effectively, or it causes toxicity due to accumulation in other tissues, it won’t succeed. “We’re always actively thinking about ways to make our molecules safer and as effective as possible,” says Tristan Maurer, Executive Director of Translational Modeling and Simulation in Medicine Design at Pfizer’s Kendall Square, Cambridge research site. “Finding therapeutic targets that are both safe and effective is perhaps one of the pharmaceutical industry’s biggest challenges. If we can do something in drug design to impact pharmacokinetics in a way that avoids safety risks associated with an otherwise promising molecular target, it potentially increases the number of targets that we can go after.”
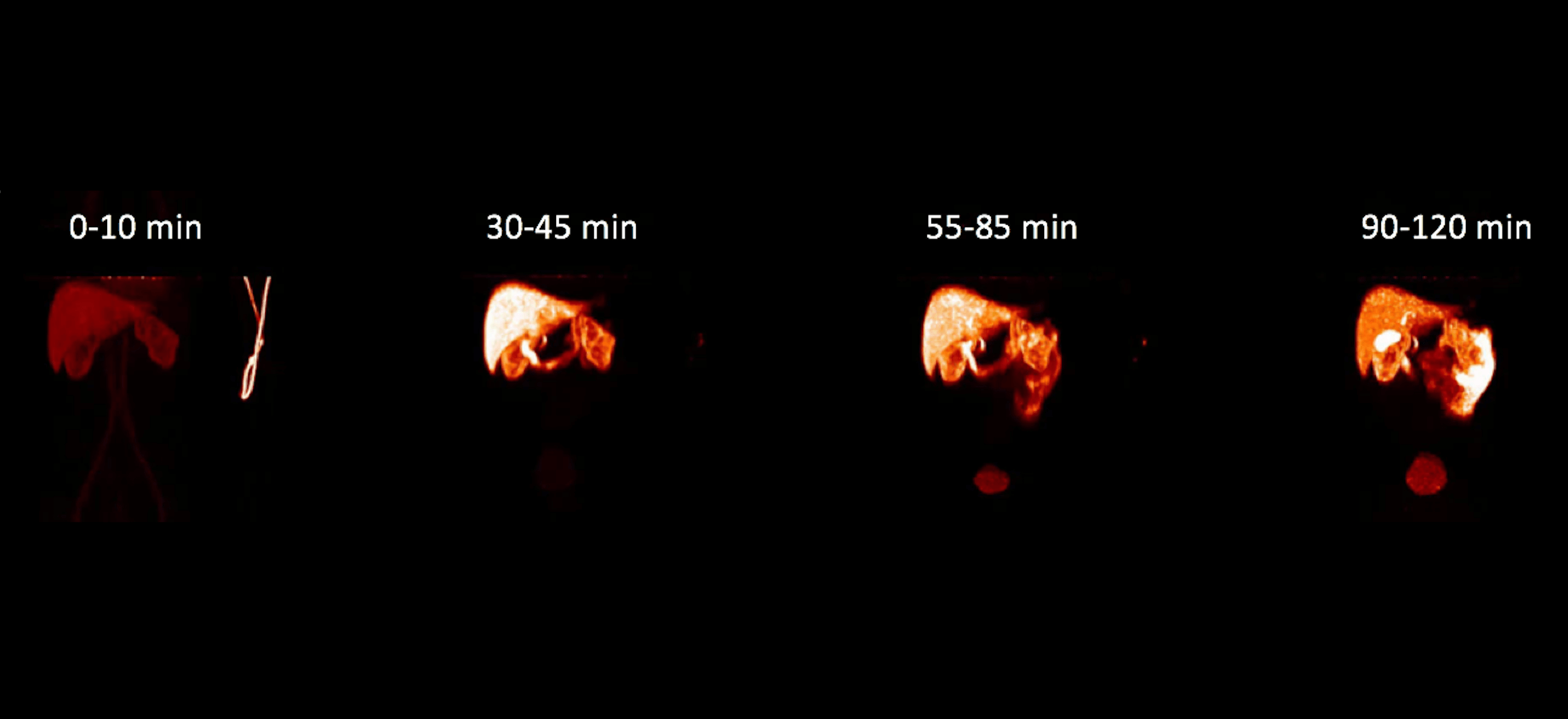
In recent years, scientists have been working to design safer and more effective drugs for NASH, an advanced form of fatty liver disease, which affects about 3 to 5 percent of people around the globe. A number of promising molecular targets for NASH are found in both the liver and other tissues. While we may want to reach these molecular targets in the liver, in some cases, we don’t want these medicines traveling to other tissues. “To be successful with these targets, we need to not only make sure the drug interacts potently with the molecular target, but also deliver the drug to the liver, make sure it sticks around long enough to have a therapeutic effect and minimize delivery to other organs. This is the essence of what we call liver targeting,” says Maurer.
Leveraging the transporters
Scientists have found success by designing drugs that exploit another feature of the liver: It has special transport proteins that are good at recognizing certain medicines and shuttling them into its cells. By harnessing these transporters, the drugs can reach their target. “By gaining a deeper understanding of transporters and how they recognize certain chemical structures, our chemists have been able to design molecules that are preferentially delivered to the liver,” says Maurer. In particular, acidic molecules are more likely to be recognized by a family of high capacity transporters in the liver, called organic anion transport proteins. Of course, delivery of a potent molecule to the liver is only the first step. Scientists also have to ensure that, once inside the liver, the drug isn’t immediately eliminated by other transporters or enzymes contained within the liver." Achieving this balancing act in design is the ultimate challenge we face in targeting drugs to the liver,” says Maurer.
Design rooted in clinical outcomes
In practice, tissue targeting is a multidisciplinary endeavor requiring expert knowledge in disease biology, safety, pharmacology, pharmacokinetics and medicinal chemistry. Ultimately, clinical success requires translating this knowledge into the drug’s design. To this end, scientists are increasingly using mathematical models to integrate diverse knowledge and explicitly align drug design efforts to a desired clinical outcome. For example, if the goal for safety and efficacy is to have a liver concentration (of the medicine) 20-times that of other tissues, the model can help identify the characteristics of the molecule (e.g. rate of uptake, transport, elimination) that are necessary to achieve this goal.
Next Horizons in tissue targeting
As complex as it is, targeting the liver via transporters is really the low-lying fruit in the broader, tissue targeting space. We are only beginning to understand transporters that could be used in other tissues. In addition, novel tools (e.g. nanoparticles, drug conjugates) that target cell surface receptors may dramatically increase the potential for tissue targeting. Finally, basic physiological properties of cells and tissues (e.g. vascular physiology, lymphatic flow, pH gradients and electrical potential) offer opportunities for tissue targeting. “This is truly an exciting area that we believe will really help us to potentially deliver safer and effective medicines to patients,” says Maurer.
